How T.J. Samson is expanding access to EEG with BrainWatch

For many smaller hospitals, consistent access to EEG remains a persistent challenge when acute neurology care is required. Limited EEG technologist availabilityi, competing demands across departments, and dependence on off-site resources often leave clinicians without timely and important diagnostic information.
This is particularly challenging for unconscious patients, or those presenting with altered mental status or suspected seizures within the emergency department (ED) where research has shown that less than 3% of ED patients with suspected seizures receive EEG confirmation within 24 hoursii. Unfortunately, time delays in diagnosis and treatment of patients with suspected seizure activity can also be exacerbated by transfers to tertiary centers for neurology diagnostics.
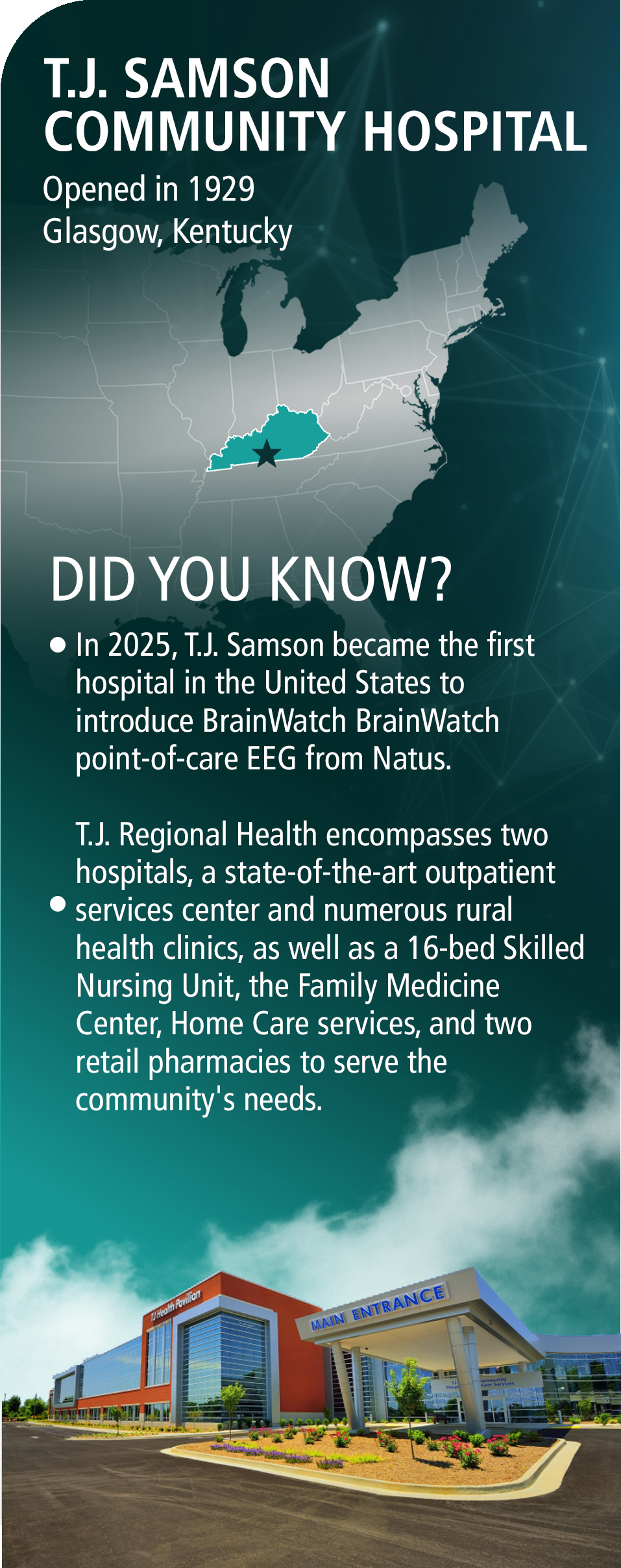
Like many regional and rural providers, T.J. Samson Community Hospital in Glasgow, Kentucky, was experiencing many of these challenges as well as an increase in patients with suspected neurological disorders like epilepsy and non-convulsive status epilepticus (NCSE). For T.J. Samson, particularly within the ED, this meant clinicians had to rely on narrow windows of neurodiagnostic availability or experienced a lack of access to EEG monitoring altogether. As a result, neurologists and ED physicians often faced difficult decisions about whether certain patients could safely remain within the hospital.
“We knew we were sending patients out simply because we didn’t have a quick, reliable way to evaluate what was happening electrically in the brain,” said Ryan Skinner, Director of Clinical Improvement at T.J. Regional Health. “It wasn’t a matter of capability. It was a matter of access.”
To bridge the gap for these acutely ill patients, Dr. Kyra Schmidt, a board-certified neurologist practicing at T.J. Samson, began exploring new point-of-care EEG (POC-EEG) tools. Her goal was not to replace traditional EEG testing, but to ensure clinicians could access the data they needed to make informed, rapid decisions during suspected neurological emergencies. Even when EEG technologists were readily available, Dr. Schmidt knew that care teams needed a way to access brain data in a faster, more frequent way. The search led Ryan Skinner and Dr. Schmidt to BrainWatch™ from Natus, a POC-EEG solution that would quickly and dramatically shift how the hospital delivers acute neurology care.
“Without 24-hour EEG, we were left with real uncertainty about the nature of the events patients were experiencing. We often had to transfer patients by default so they could access readily available EEG. We had providers ready to care for them, but didn’t have the technology to diagnose in a timely fashion,” said Dr. Schmidt. “BrainWatch has changed that. We’re now catching clear seizures we previously did not have such rapid visibility into. It has directly changed our time to diagnosis, helped us avoid unnecessary transfers, and substantially changed patient outcomes. It is giving me clinical information I didn’t have access to before.”
Shortages in the number of skilled EEG technologists in the United States are a recognized issue, but the challenge is especially acute for smaller community and rural providersiii. Like other hospitals of its kind, T.J. Samson shares a small team of EEG technologists across neurology care and sleep services, with even more limited access during weekends and holidays. Before BrainWatch, patients often faced delays of up to 12 hours or more before traditional EEG could begin.
“At best, we can order a formal EEG and have it done in 4 to 6 hours,” said Dr. Schmidt. “Realistically, it may be up to 12 hours if it is during off-hours or at night. And in acute neurology, those hours matter an awful lot.”
This made the introduction of BrainWatch particularly timely. POC-EEG gives clinicians and other care professionals immediate insight into potential neurological events. As a result, they can rule out or confirm the presence of seizure activity, non-convulsive status epilepticus (NCSE), and other neurological conditions much earlier in the care process.
After evaluating different diagnostic approaches and tools, the team at T.J. Samson chose BrainWatch based on three important factors:

First, BrainWatch offered fast deployment and time to EEG without the need for adding staff or lengthy training. Nurses, respiratory therapists, and other care providers needed technology that was easy to learn and did not disrupt their normal routines and workflows.
Next, BrainWatch leverages Natus’ industry-leading NeuroWorks® EEG software interface which Dr. Schmidt already knew well. BrainWatch EEG data is available in a secure, web-based portal, offering fast and convenient remote access with full NeuroWorks functionality while still displaying the EEG in the same format, scale, and orientation she was accustomed to.
“The BrainWatch workflow felt familiar and the signal quality has been impressive,” she said. “With some other point-of-care systems, it’s almost like you are translating too many things with different EEG and web services. With BrainWatch, I see the EEG waves as I always see the EEG waves, in the specific pattern and size and orientation that they’re normally in and all the buttons are in the right place.”
Third, BrainWatch was easy to implement without changing workflows or straining the already limited neurodiagnostic workforce. “Natus’ POC-EEG technology offered a tool our clinicians could trust, but it also needed to be something we could easily operationalize,” said Ryan Skinner. “For us, BrainWatch checks both those boxes.”
Both Dr. Schmidt and Ryan Skinner noted that these factors and contributed to the rapid adoption of the new tool within the T.J. Samson emergency department, which is now spreading to the ICU and other patient floors as well.

After the decision to deploy and staff training was conducted, BrainWatch exceeded expectations almost immediately. Instead of waiting many hours or triggering transfers for traditional EEG monitoring, the care team could request the BrainWatch headband and obtain actionable data in 10–15 minutes
“That kind of turnaround simply didn’t exist for us before,” Dr. Schmidt said. “It changes how quickly I can determine whether a patient is having a seizure, especially when it comes to suspected NCSE. It’s common sense that this type of speed translates directly into better neurological care.”
As an example, Dr. Schmidt describes a striking patient case early after BrainWatch was introduced when a young patient arrived in the ED after a seizure-like event. Before we had point-of-care EEG, this patient was transferred to under go 24-hour EEG monitoring at a tertiary center, which returned normal results, even though her symptoms persisted for days. This included a prolonged period where the patient struggled to speak or respond clearly. With no EEG evidence of seizures at that time, the event was considered possibly non-epileptic and the patient came off seizure medication.
“EEGs only tell you what’s going on right then. So, even in patients I know have uncontrolled epilepsy, a random EEG may be normal unless we catch the neurological event right during or right after the event itself,” noted Dr. Schmidt.
After a few months, the patient returned to the ED after a similar episode and the team applied BrainWatch immediately. Although the patient showed no obvious convulsive activity, the EEG began streaming within minutes, revealing multiple right-temporal focal seizures. Dr. Schmidt noted that they were able to confirm that this patient does have epilepsy. Because the seizures were confirmed so quickly with BrainWatch, the team was able to initiate appropriate medication, stabilizing the patient’s condition and remove the need for a transfer for neurological insight. Today, the patient remains episode-free, with a better understanding of their diagnosis and the need to continue treatment.
“Because we were able to access data so quickly with BrainWatch, the patient received treatment right away, and their clinical course changed because we caught something that would have otherwise remained invisible,” Dr. Schmidt said. “It reinforced how BrainWatch complements traditional EEG.”
Before BrainWatch, many patients with altered mental status or suspected seizures were transferred to other providers for neurology care as a precaution. With no EEG immediately available, ruling out non-convulsive seizures or status epilepticus was next to impossible. As a result, patients were often transferred to larger facilities where traditional EEG was more readily available.
“Every time we sent a patient out for something we couldn’t diagnose locally; we risked losing not only that encounter but every future one,” Ryan Skinner explained. “Transfers disrupt care, fragment our patient relationships, and result in additional stress for patients and their families.”
For T.J. Samson, BrainWatch has dramatically changed those dynamics. More than half of the early cases where the new POC-EEG technology was used involved patients who previously would have been transferred solely due to lack of EEG access. With immediate diagnostic insights, however, clinicians could confidently continue care in-house, maintaining continuity of care and improving follow-up statistics.
“BrainWatch has become an important bridge technology for us,” Ryan Skinner stated. “It keeps patients home when they can safely stay here, and it gives our clinicians the confidence to make that call.”
Although BrainWatch was first introduced to support emergency neurology care, its impact at T.J. Samson has quickly spread across the hospital. On evenings and weekends, when access to traditional EEG is limited, some clinicians began using BrainWatch to prioritize neurological concerns among inpatients. In several cases, that faster clarity helped speed discharges and reduce prolonged ED holds.
With physician communication and workflows established early, adoption moved quickly and Ryan Skinner attributes much of the expansion to nurses, respiratory therapists, and other staff members who embraced BrainWatch right away. “Our care teams embraced it without hesitation,” Skinner said. “Their immediate comfort with the technology and the ease with which BrainWatch has been incorporated into our workflows are major reasons adoption is happening so fast.”
Dr. Schmidt adds that BrainWatch “…. has allowed me to get clinical answers where I would not have otherwise been able to obtain them. When a patient arrives unconscious, or with an active episode, I can get a quick clinical judgement immediately, from whether we need to treat for seizures, or if that patient needs a transfer. BrainWatch gives me clinical information I didn’t have access to before.
As word spreads, more T.J. Samson clinicians and nurses are requesting BrainWatch whenever neurological changes such as seizures and NCSE are suspected. While Dr. Schmidt continues to guide the appropriate use of POC-EEG technology, she sees the enthusiasm as a sign of growing clinical alignment. “Our teams know that BrainWatch provides answers when they’re needed most,” she said. “That alone accelerates trust and ultimately improves patient care.”
The success of BrainWatch is now shaping broader neurology planning at T.J. Samson Community Hospital. Dr. Schmidt expects it to play a growing role in complex ICU evaluations, particularly for patients whose neurological conditions progress rapidly. “This is the type of innovation community hospitals truly need,” Dr. Schmidt said. “BrainWatch doesn’t replace comprehensive EEG, it expands the potential for comprehensive neurology care for hospitals like ours.”
In a very short time, BrainWatch has become a trusted supplement to traditional EEG, filling access gaps that once caused dangerous diagnostic delays or forced transfers. In this way, T.J. Samson Community Hospital is proof that advanced neurology care doesn’t have to be limited by geography or resource shortages. By choosing BrainWatch, the community hospital has demonstrated what’s possible when strong leadership and advanced technology come together to deliver the highest level of patient care, close to home.
052235 RevA