
While brain function has not historically been considered one of the continuously monitored vital signs within the ICU, electroencephalography (EEG) use in the ICU has risen significantly as more advanced neurocritical care concepts emerge. We know that untreated brain damage can seriously impact ICU patients’ neurological integrity and, for many people, can be the difference between life and death. In addition, patients in the ICU are often sedated or even paralyzed, making it difficult to assess their neurological status using traditional methods such as clinical examinations and bedside tests.
EEG provides a unique window into brain activity, allowing healthcare professionals to monitor patients’ neurological status in real time. Patients suffering from traumatic brain injury (TBI), stroke and/or cardiac arrest receive significant benefits from continuous EEG monitoring as, for these patients, early detection and fast treatment can be crucial. By continuously monitoring brain activity, EEG allows healthcare professionals to make informed decisions about patient care and reduce the risk of an initial secondary brain injury. This can result in a faster recovery and a shorter length of stay in the ICU, which in turn helps reduce costs and, most importantly, improves patient outcomes.
Leading associations worldwide agree with this assessment. For example, the European Society of Intensive Care Medicine has stated that continuous EEG monitoring is a valuable tool for diagnosing specific indications. Additionally, the American Clinical Neurophysiology Society has recommended guidelines for the use of EEG monitoring in the ICU, including:
TBI can result in a wide range of neurological complications, including secondary brain injury resulting from hypoxia, hypotension, and elevated intracranial pressure. EEG provides continuous monitoring of brain activity, enabling healthcare professionals to detect changes in the brain’s electrical activity that may indicate the onset of secondary brain injury. This allows for early intervention and the initiation of appropriate treatments, which can improve patient outcomes and reduce the risk of long-term neurological complications.
EEG monitoring provides different types of advanced analysis of brain activities via EEG trending for TBI patients or at high risk, including those experiencing stroke or cardiac arrest, amongst others. These trending analyses allow gradual and dynamic changes in the EEG to be identified sooner by ICU personnel, thus predicting possible secondary brain insult and intervene accordingly.
The consequences of TBI can be temporary altered mental status, loss of consciousness, awareness, and memory. Undetected TBI can cause permanent neurological damage and even death. Simply put, EEG monitoring in the ICU can help prevent potentially life-threatening events for patients with diagnosed TBI or at high risk.
According to the CDC, heart disease cost the United States about $229 billion each year from 2017 to 2018. This includes the cost of healthcare services, medicines, and lost productivity due to death. One person in the US has a heart attack every 40 seconds.[CDC] The use of EEG monitoring for cardiac arrest patients in the ICU is becoming increasingly recognized as a valuable tool for managing these patients as they recover, particularly in the critical first hours and days of hospitalization.
One of the main benefits of using EEG in the ICU for cardiac arrest patients is the early detection of brain injury. Cardiac arrest can result in a lack of oxygen to the brain, leading to brain damage and potential long-term neurological complications.
As stated earlier, EEG provides data that allows healthcare professionals to detect changes in the brain’s electrical activity that may indicate the onset of brain injury. This allows for early intervention and the initiation of appropriate treatments, which helps reduce the risk of long-term neurological complications that may go undetected during traditional vital signs monitoring and neurological examinations.
According to the CDC, heart disease cost the United States about $229 billion each year from 2017 to 2018. This includes the cost of healthcare services, medicines, and lost productivity due to death. One person in the US has a heart attack every 40 seconds.[CDC] The use of EEG monitoring for cardiac arrest patients in the ICU is becoming increasingly recognized as a valuable tool for managing these patients as they recover, particularly in the critical first hours and days of hospitalization.
One of the main benefits of using EEG in the ICU for cardiac arrest patients is the early detection of brain injury. Cardiac arrest can result in a lack of oxygen to the brain, leading to brain damage and potential long-term neurological complications.
As stated earlier, EEG provides data that allows healthcare professionals to detect changes in the brain’s electrical activity that may indicate the onset of brain injury. This allows for early intervention and the initiation of appropriate treatments, which helps reduce the risk of long-term neurological complications that may go undetected during traditional vital signs monitoring and neurological examinations.

Along with its diagnostic and monitoring applications, EEG in the ICU can also be used to guide the administration of sedatives and anesthesia, which are often necessary to manage the symptoms of stroke, the impacts of traumatic brain injuries, and for patients recovering from cardiac arrest. These medications can have adverse effects on the brain and impair recovery, and EEG provides continuous monitoring of the brain’s electrical activity, allowing healthcare professionals to adjust the dose of sedatives and anesthesia to minimize their adverse effects and improve patient outcomes.
Seizures are also a common symptom of TBI, cardiac arrest, and stroke, and can cause further brain injury and impair recovery, making early detection and treatment crucial for improving patient outcomes. EEG monitoring provides a continuous and objective assessment of the brain’s electrical activity, allowing healthcare professionals to detect seizures in real-time and initiate appropriate treatment. Without EEG monitoring, seizures may go unnoticed or occur without warning, causing potentially negative impacts to a patient’s prognosis.
Despite its benefits, many healthcare professionals perceive EEG as a complex and time-consuming technology that requires specialized training and expertise. In addition, different EEG systems and analysis methods can produce different results, leading to uncertainty about the results of EEG monitoring. Concerns around patient comfort and other aspects of EEG monitoring can contribute to a reluctance to introduce this potentially life-saving tool in the ICU.
Another reason for resistance to using EEG in the ICU is the perception that it is not a “necessary” technology. Some healthcare professionals believe that traditional methods, such as clinical examination and bedside tests, are sufficient for assessing a patient’s neurological status. This can lead to a perception that EEG is an unnecessary expense and an additional burden on the already limited resources of the ICU.
Additionally, some healthcare professionals may resist using EEG in the ICU due to concerns about patient comfort. EEG requires the attachment of electrodes to the scalp, which can be uncomfortable for patients and may interfere with their ability to rest and recover. There may also be concerns about the privacy of patient data and the potential for the unauthorized use of EEG results.
Finally, there may be resistance to using EEG in the ICU due to the lack of standardization in EEG monitoring and analysis methods. Different EEG systems and analysis methods can produce different results, making it difficult to compare EEG readings between patients and across different healthcare facilities. This can lead to confusion and uncertainty about the results of EEG monitoring and may discourage healthcare professionals from using EEG in the ICU.
Fortunately, advanced technology exists, such as EEG trending that can help simplify EEG analysis and provide ways for even those healthcare professionals new to EEG to understand easily and incorporate this important monitoring tool into their ICU. With support from their neurodiagnostic and neurology team, ICU personnel can gain confidence in using EEG monitoring for their high-risk patients
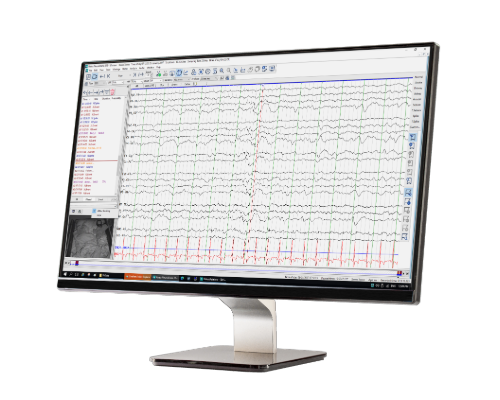 Natus solutions like NeuroWorks® EEG Software, BRAIN QUICK ICU and Moberg CNS simplify collecting, monitoring, trending, and managing data for cEEG ICU monitoring. NeuroWorks systems are scalable to meet the needs of private practice clinics, hospitals, large teaching facilities and EEG service providers. Natus NeuroWorks is a cutting-edge, single solution for EEG use in the ICU, exhibiting advanced software for clinical excellence.
Natus solutions like NeuroWorks® EEG Software, BRAIN QUICK ICU and Moberg CNS simplify collecting, monitoring, trending, and managing data for cEEG ICU monitoring. NeuroWorks systems are scalable to meet the needs of private practice clinics, hospitals, large teaching facilities and EEG service providers. Natus NeuroWorks is a cutting-edge, single solution for EEG use in the ICU, exhibiting advanced software for clinical excellence.
SOURCES
ACNS. (n.d.). American Clinical Neurophysiology Society. Guidelines and consensus statements. https://www.acns.org/practice/guidelines
Centers for Disease Control and Prevention. (2022, October 14). Heart disease facts. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/facts.htm
Claassen, J., Vespa, P., & Participants in the International Multi-disciplinary Consensus Conference on Multimodality Monitoring (2014). Electrophysiologic monitoring in acute brain injury. Neurocritical care, 21 Suppl 2, S129–S147. https://doi.org/10.1007/s12028-014-0022-8
Westhall, E., Rossetti, A. O., van Rootselaar, A. F., Wesenberg Kjaer, T., Horn, J., Ullén, S., Friberg, H., Nielsen, N., Rosén, I., Åneman, A., Erlinge, D., Gasche, Y., Hassager, C., Hovdenes, J., Kjaergaard, J., Kuiper, M., Pellis, T., Stammet, P., Wanscher, M., Wetterslev, J., … TTM-trial investigators (2016). Standardized EEG interpretation accurately predicts prognosis after cardiac arrest. Neurology, 86(16), 1482–1490. https://doi.org/10.1212/WNL.0000000000002462
043572 RevA