Guide to support sleep apnea patients from PSG sleep study to treatment

Sleep is a vital component of every person’s overall health and well-being as it affects important body functions including energy conservation, restitution of autonomous functions, memory consolidation, regulating immune system, and brain restoration. Consequently, insufficient sleep duration and poor sleep quality due to sleep apnea can lead to significant cardiovascular issues such as high blood pressure, heart attack, and stroke.
In this guide, you can explore the medical procedures that can help you support the patient journey: from symptoms of sleep disorders, polysomnography studies, diagnosing sleep apnea, and treatment for patients. This guide includes:
⇒ What are the different types of sleep apnea?
⇒ What are the symptoms of sleep apnea?
⇒ Diagnosing sleep apnea with polysomnography
⇒ Polysomnography findings in OSA patients
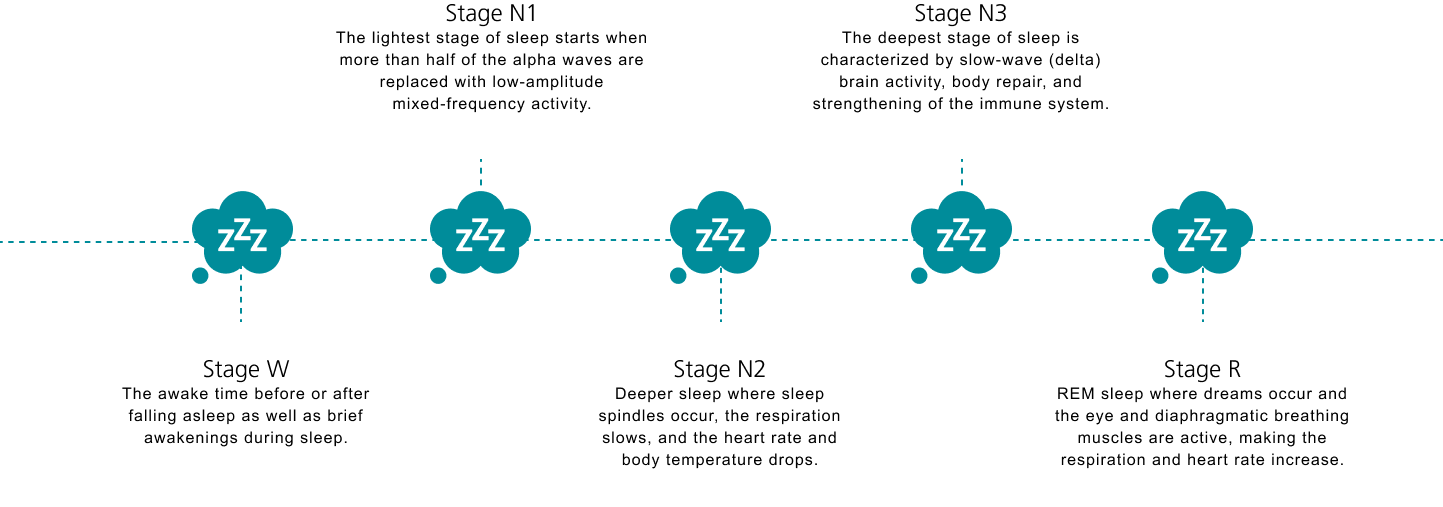
Sleep is a reversible behavioral state of perceptual disengagement from and unresponsiveness to the environment. Sleep is divided into five stages: Wake, N1, N2, N3, and rapid eye movement (REM) sleep. A person usually progresses through the stages N1-N3 of non-rapid eye movement sleep before entering REM sleep.
This takes about one to two hours after falling asleep. The cycle is repeated three to four times each night, and the majority of an adult’s sleep is spent in the N2 stage.
Sleep-related breathing disorders are characterized by abnormal respiration during sleep and are categorized into four different types:
Sleep movement disorders cause movement during or prior to sleep, which can make it difficult to fall asleep or stay asleep. Sleep movement disorders include:
Narcolepsy involves excessive daytime sleepiness and can cause uncontrollable sleep attacks to happen in the middle of any activity including eating, walking or driving.
Idiopathic hypersomnia causes patients to be excessively sleepy during the day even after a good or prolonged night’s sleep. Like narcolepsy, the need to sleep can strike at any time of the day, which can be dangerous if the patient is driving.
Parasomnias are types of disturbing events or experiences that can happen just before patients fall asleep, while they are sleeping, or as they are waking up. The events include:
REM sleep behavior disorder is a type of parasomnia where patients act out vivid dreams as they sleep by shouting, swearing, punching, kicking or even jumping.
Circadian rhythm disorders are disruptions in a patient’s internal clock that regulates a variety of biological processes, which makes it difficult to follow normal sleep patterns. The circadian rhythm disorders include:
Insomnia involves difficulty falling asleep, difficulty staying asleep throughout the night and can include daytime symptoms. There are two types of insomnia:
Source: http://sleepeducation.org/sleep-disorders-by-category
Central sleep apnea (CSA) occurs when the body does not respond to the cues from the brain’s system for controlling muscles involved in respiration, leading to slower and shallower breathing. There are different types of central sleep apnea, including CSA due to Cheyne-Stokes breathing, high-altitude periodic breathing, medical or neurological condition without Cheyne-Stokes breathing. Obstructive sleep apnea (OSA) is the most common type of sleep related breathing disorders when diagnosing sleep apnea. Recent studies have shown that 1 in 5 adults across the globe have obstructive sleep apnea, and that the prevalence of OSA is likely to continue to increase over time due to demographic and other factors.
Obstructive sleep apnea (OSA) is the most common type of sleep related breathing disorders. Recent studies have shown that 1 in 5 adults across the globe have OSA, and that the prevalence of OSA is likely to continue to increase over time due to demographic and other factors.
Obstructive sleep apnea is characterized by recurrent episodes of complete or partial upper airway collapse during sleep due to different causes like:
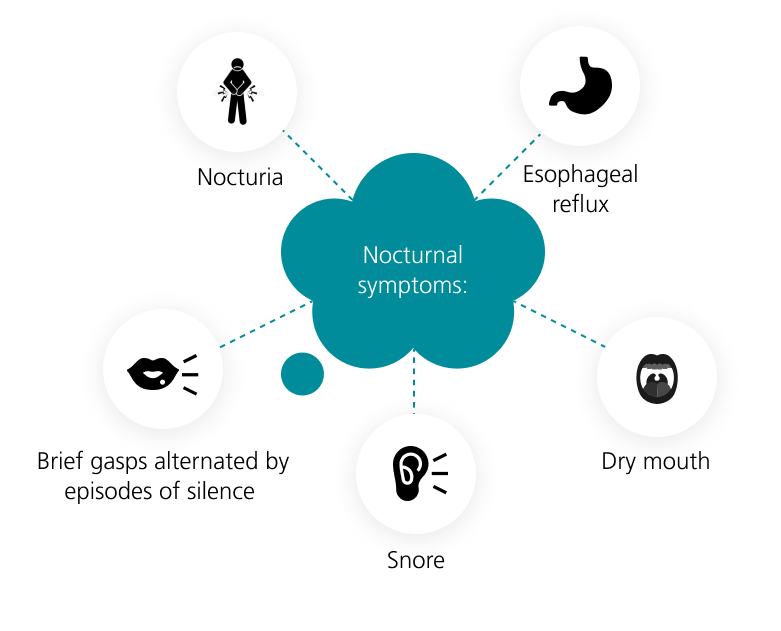
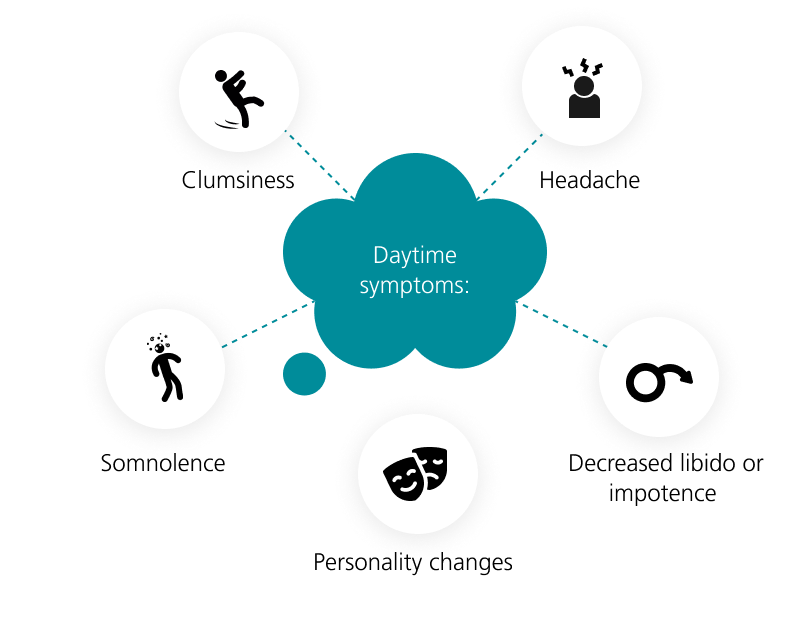
Sleep apnea symptoms can be categorized by nocturnal symptoms and daytime symptoms. Some primary sleep apnea symptoms include:
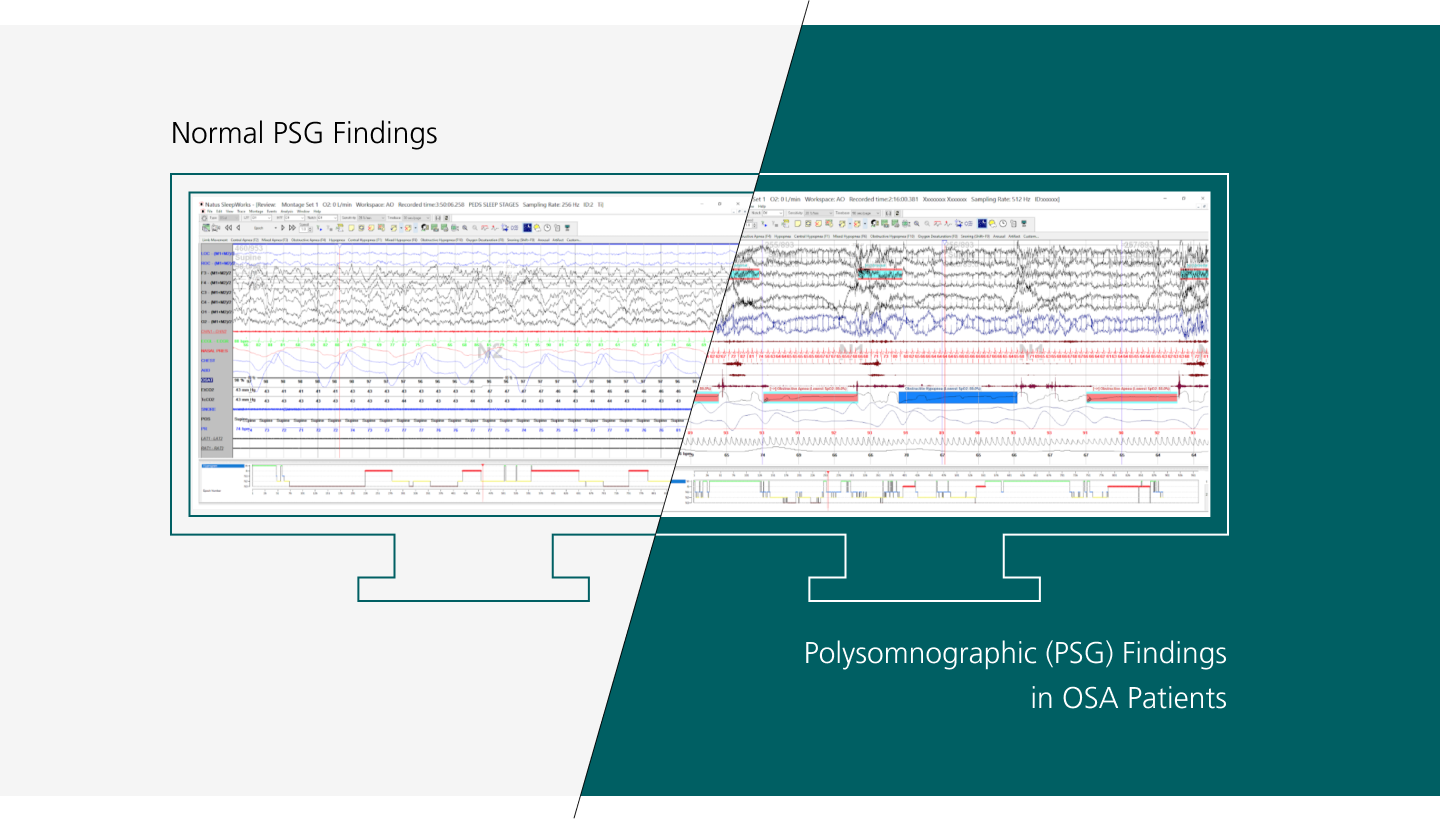
Diagnosing sleep apnea will usually require polysomnography (PSG), also known as a sleep study. PSG is the most commonly used test for diagnosing sleep apnea, especially in the diagnosis of obstructive sleep apnea. PSG measures several sleep variables, including apnea-hypopnea index (AHI) which is the sum of apneas (complete obstruction of upper airway collapse) and hypopneas (partial obstruction) per hour of sleep.
Apnea is defined as the absence of airflow for more than 10 seconds, and hypopnea is reduction in respiratory effort with more than 4% oxygen desaturation. An AHI of more than five events per hour of sleep is considered abnormal and the patient is considered to have a sleep disorder.
Diagnosing sleep apnea patients sleep test medical procedures which may include both unattended sleep monitoring and attended PSG sleep studies There are several levels of PSG sleep studies and classifications as per AASM based on the recorded channels.
A Level 1 PSG sleep study is done overnight in a sleep lab or hospital. The study is used to help determine the cause of excessive daytime sleepiness and to diagnose various sleep disorders.
Level 1 sleep study requirements:
Level 2 PSG sleep study records brain waves, heartbeats, and breathing as the patient sleeps. It also charts eye movements, limb movements, and oxygen in the blood.
Level 2 attended in-lab PSG requires a minimum of seven channels:
A Level 2 PSG sleep study can also be done at the patient’s home with a portable, unattended PSG. This also requires recording from a minimum of seven channels in the sleep study equipment being used:
A Level 3 PSG sleep study is conducted in the patient’s home. The device provided records oxygen levels, heart rate, airflow, snoring, and other parameters while the patient is asleep. Level 3 PSG sleep study with a portable, unattended PSG requires a minimum of four channels:
A Level 4 PSG sleep study refers to sleep apnea screening with oximetry, which measures blood oxygen levels and may also include measuring heart rate. Level 4 PSG sleep studies are usually used to test for pediatric sleep disorders.
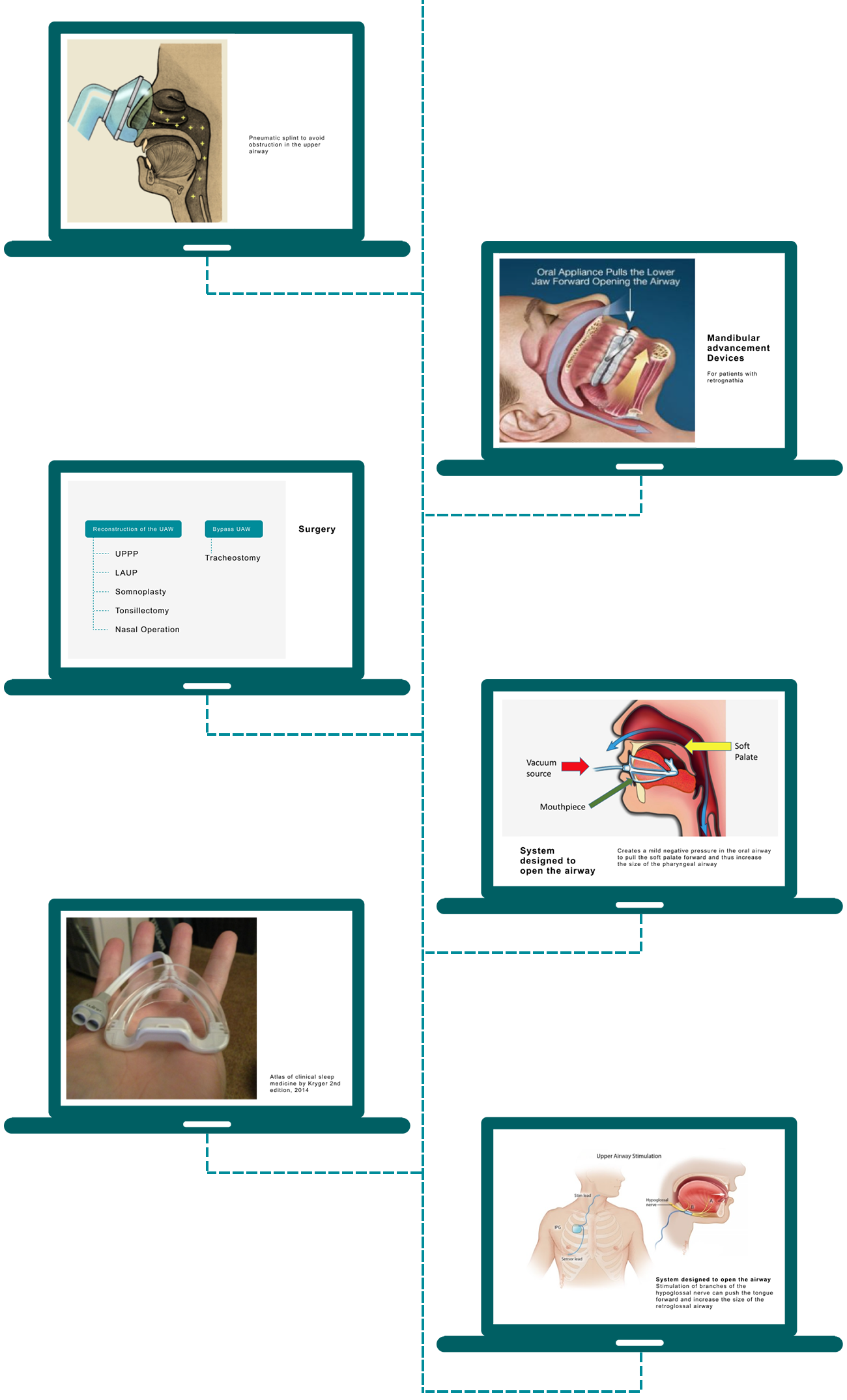
After diagnosing sleep apnea in a patient, the proper device for treating sleep apnea must be selected. Some options for treating sleep apnea patients include:
Continuous Positive Airway Pressure (CPAP): This device includes a mask that the patient wears over his or her nose, which serves as a pneumatic split for the upper airway to avoid obstruction.
Mandibular advancement device: For patients with retrognathia, this oral device keeps his or her tongue from blocking the throat by bringing the lower jaw forward.
System designed to open the airway: This device creates a mild negative pressure in the oral airway to pull the soft palate forward and thus increase the size of the pharyngeal airway.
Upper airway stimulator: This is a small implanted device that senses breathing patterns and delivers mild stimulation of branches of the hypoglossal nerve that can push the tongue forward and increase the size of the retroglossal airway.
Surgery: For patients who have a deviated nasal septum, swollen tonsils, and adenoids, or a small lower jaw that causes the throat to be too narrow, surgery like somnoplasty, UPPP, LAUP, tonsillectomy or nasal operation can help.
035383 RevB