
A tinnitus assessment is the second piece of the larger tinnitus evaluation for audiologists, following a standard hearing assessment. This provided overview focuses on specific tinnitus tests, which go beyond a standard audiological hearing evaluation, to obtain a clear and complete clinical picture of the tinnitus patient. For a more detailed look into the additional components of a tinnitus evaluation, visit The Tinnitus Toolbox.
A specific assessment for tinnitus following an initial hearing assessment consists of subjective measurements, objective measurements and psychoanalytic questionnaires which aim to quantify tinnitus symptoms and to provide insight into the impact of these symptoms on the quality of life for the tinnitus patient. This step also helps audiologists classify tinnitus: subjective vs. objective (pulsatile) tinnitus, primary vs. secondary tinnitus, acute vs. chronic tinnitus and bothersome vs. non-bothersome tinnitus.
Tinnitus is frequently associated with auditory conditions, such as hearing loss and hyperacusis, but is also associated with nonauditory conditions including stress, anxiety, depression and insomnia.
Looking to learn more about bothersome tinnitus management? Download our white paper here.
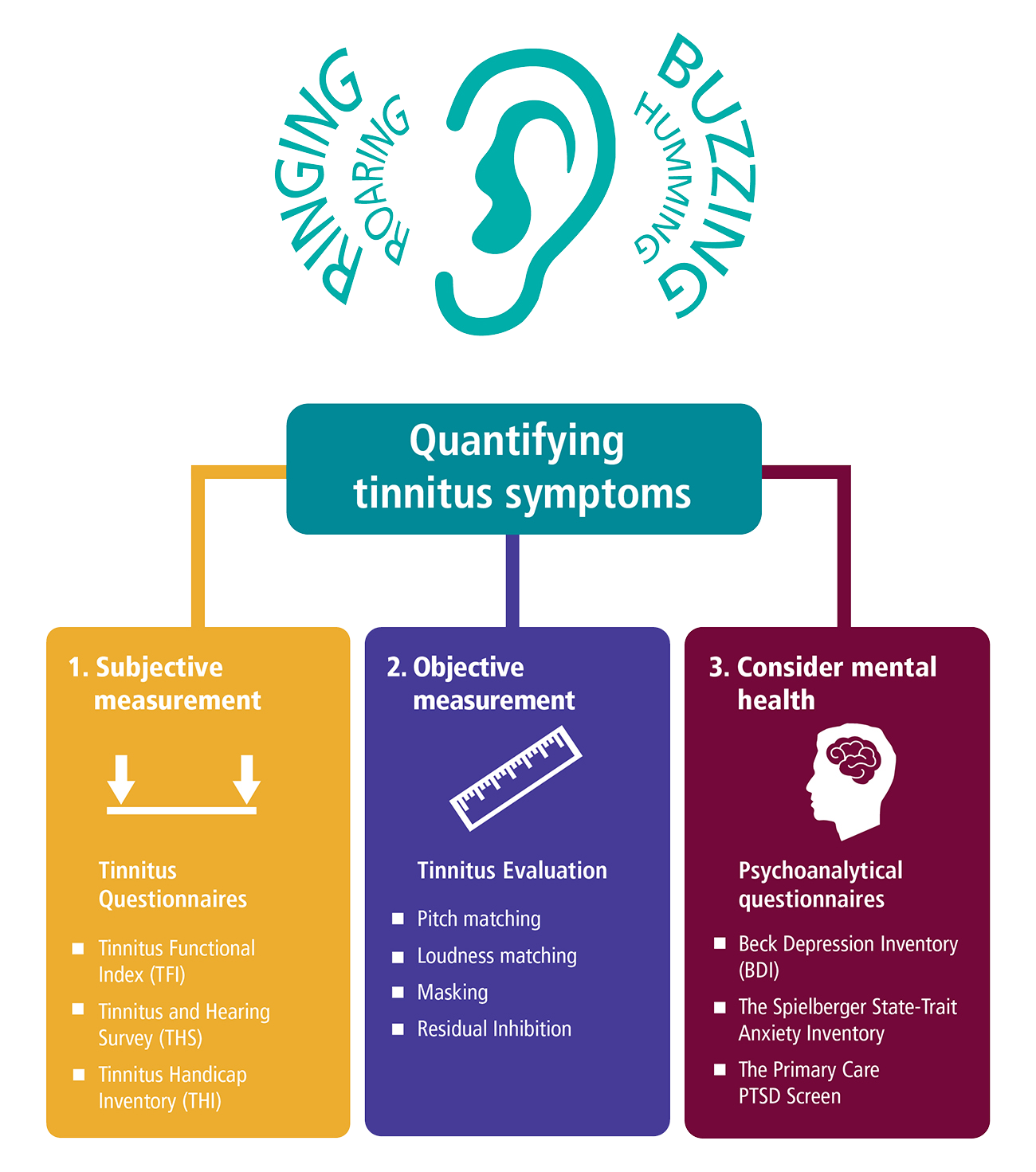
A tinnitus assessment protocol includes tools and questionnaires for the evaluation of tinnitus reaction and distress in the tinnitus patient. Three tools for subjective tinnitus assessment include the Tinnitus Handicap Inventory (THI) and Tinnitus Functional Index (TFI), which evaluate and scale the severity and negative impact of tinnitus on the patient1 and the Tinnitus and Hearing Survey (THS), a tool to differentiate potential hearing problems from tinnitus problems.2 Additionally, these tinnitus assessment tools are used to measure progress with tinnitus treatment and management outcomes.
“
The Tinnitus and Hearing Survey is a great clinical tool used to identify patients attributing their communication difficulties onto their tinnitus rather than their hearing deficit.
Dany Pineault, AuD
A second step for tinnitus assessment audiology is to better define the auditory attributes of the tinnitus patient in terms of perceived pitch, loudness and maskability with external sounds. The psychoacoustic measures for these key tinnitus indicators are comprised of pitch and loudness matching procedures, minimum masking level testing and residual inhibition testing. Tinnitus pitch and loudness matching procedures are critical when prescribing amplification for this population as research shows greater benefits with hearing aids for tinnitus patients when their psychoacoustic attributes fall within the instrument’s frequency bandwidth.3,4
Psychoanalytical questionnaires are a last step in a tinnitus assessment which help you to identify any emotional distress encountered by patients with tinnitus symptoms. Some of the most common mental health problems associated with bothersome tinnitus are depression, anxiety disorders, sleep disorders and post-traumatic stress disorder.
The Beck Depression Inventory, The Spielberger State-Trait Anxiety Inventory and the Primary Care PTSD Screen are clinical tools with easy and rapid scoring instructions to measure any negative reaction from symptoms. Having a more complete understanding of a tinnitus patient’s psychological well-being is crucial for developing the appropriate tinnitus management strategy and improving the quality of life for your patient. The therapeutic value of counseling for patients with tinnitus is well-established and is one of the most important components of all audiological interventions.5,6
To learn more about tinnitus management and treatment opportunities, watch Dr Hashir Aazh’s lecture entitled, “Audiologist-Delivered CBT for Tinnitus, Hyperacusis and Misophonia”.
Sources:
1. Meikle, M. B., Henry, J. A., Griest, S. E., Stewart, B. J., Abrams, H. B., McArdle, R., Myers, P. J., Newman, C. W., Sandridge, S., Turk, D. C., Folmer, R. L., Frederick, E. J., House, J. W., Jacobson, G. P., Kinney, S. E., Martin, W. H., Nagler, S. M., Reich, G. E., Searchfield, G., … Vernon, J. A. (2012). The Tinnitus Functional Index: Development of a New Clinical Measure for Chronic, Intrusive Tinnitus. Ear &; Hearing, 33(2), 153–176. https://doi.org/https://www.ncrar.research.va.gov/Education/Documents/TinnitusDocuments/TFI_EarHearing_2011.pdf
2. Henry, J. A., Griest, S., Zaugg, T. L., Thielman, E., Kaelin, C., Galvez, G., & Carlson, K. F. (2015). Tinnitus and hearing survey: a screening tool to differentiate bothersome tinnitus from hearing difficulties. American journal of audiology, 24(1), 66–77. https://doi.org/10.1044/2014_AJA-14-0042
3. McNeill, C., Tavora-Vieira, D., Alnafjan, F., Searchfield, G.D. & Welch, D. (2012). Tinnitus pitch, masking, and the effectiveness of hearing aids for tinnitus therapy. International Journal of Audiology; 51: 914-919. 32.
4. Araujo Tde, M. & Iorio, M.C. (2015). Effects of sound amplification in selfperception of tinnitus and hearing loss in the elderly. Brazilian Journal of Otorhinolaryngology; 82(3):289-296
5. American Speech-Language-Hearing Association. Guidelines for audiologists providing informational and adjustment counseling to families of infants and young children with hearing loss birth to 5 years of age (guidelines), 2008; www.asha.org/policy on 20.07.09
6. Aazh H, Moore BC, Lammaing K, Cropley M. Tinnitus and hyperacusis therapy in a UK National Health Service audiology department: Patients’ evaluations of the effectiveness of treatments. Int J Audiol. 2016 Sep;55(9):514-22
040608 RevB