
The human eyes are our window to the world around us. However, most people do not realize the importance of protecting our eyes until they experience visual impairment. As our vision develops over several years during childhood and fully matures around age seven1, it is critical to diagnose and treat pediatric eye problems as early as possible.
In this article, you will learn about the most common pediatric retinal diseases in newborns and how they can be detected effectively by using digital eye imaging systems.
Our vision originates in the retina2, which is a thin layer of tissue on the back of the eye that detects light and color. In normal vision, the retina contains photoreceptors known as rods and cones that convert light into electrical impulses which are transported to the brain via the optic nerve. The brain then processes the impulses as visual information like pictures in a camera.
There are several kinds of retinal disorders but the commonality is damage to the retinal tissue causing a disruption in the transmission of information from the photoreceptors to the brain. It can result in progressive, sometimes blinding vision loss if not properly detected and treated by Ophthalmic specialists.
Retinal disorders in children can be very different than those in adults, and there are various considerations that apply specifically to the management of pediatric retina patients. In the following section, we will explore the most common pediatric retinal diseases in newborns.
1. Retinoblastoma
Retinoblastoma (image 2) is a type of eye cancer where cancer cells form in the retina of one eye or both eyes (Image 2). Retinoblastoma most commonly affects infants and young children but rarely occurs in children older than six.
The average age of children diagnosed with retinoblastoma is two years old, however some children may be born with tumors. Retinoblastoma is a rare cancer that accounts for about 2% of childhood cancers. According to the American Cancer Society nearly 200 to 300 children are diagnosed with retinoblastoma each year in the United States3.

Causes of retinoblastoma
Retinoblastoma is caused by DNA changes (genetic mutations) of the nerve cells in the retina. These mutations cause the cells to continue growing and multiplying when healthy cells would die. This accumulating mass of cells forms a tumor.
Each cell normally has two RB1 tumor suppressor genes that control how fast cells grow and cause cells to die at the right time. With at least one functioning RB1 gene, the retinal cell will not form a retinoblastoma. However, if both of the RB1 genes have mutated, the cell can grow uncontrolled leading to further gene changes, which may cause cells to become cancerous. The RB1 mutation can either occur in all the cells of the body or only in one cell in one eye:4
Symptoms of retinoblastoma
Retinoblastoma is often detected because a child’s eye looks unusual. Typically, when light enters the eye, the retina will reflect a small amount of light back through the pupil. Because of the blood vessels in the back of the eye, the light reflected has a reddish color, known as a red reflex. Abnormalities in the retina can cause either a lack of red reflex or a white pupillary reflex, also called leukocoria.7
Less common signs and symptoms of retinoblastoma can include8:
2. Retinopathy of prematurity
Retinopathy of Prematurity (ROP) is a retinal disease that can affect infants born before term. The retina does not fully develop in these preterm infants and abnormal development of weak retinal blood vessels can lead to visual impairments.
According to The National Eye Institute, 14,000 –16,000 infants are affected by some degree of ROP each year in the United States. About 90% of these cases are considered mild and as the disease improves the infants do not need treatment.
However, in severe cases infants may develop retinal detachment (image 3), where the retina separates from the layer of blood vessels that provides it with oxygen and nutrients, and if left untreated could result in blindness. For this reason, premature babies are carefully screened in hospital NICUs for ROP.9
Learn how the ROP screening process on neonates can be optimized with eye imaging in this article.

Causes of retinopathy of prematurity
There is uncertainty as to what causes ROP. However, a low birth weight and how early a baby is born are considered factors contributing to the risk of ROP. The blood vessel growth is nearly complete when a baby is born full-term as the retina finishes developing a few weeks to a month after birth. If a baby is born before term, and the blood vessels have not yet reached the edges of the retina, normal vessel development may stop.10
Symptoms of retinopathy of prematurity
In severe cases of ROP, infants might develop visible symptoms, such as leukocoria, nystagmus (abnormal eye movements), and strabismus (crossed eyes). But as most signs of ROP occur deep inside the eye, they are not easily detected and can usually only be spotted by an Ophthalmologist examining the baby’s retina.11
3. Congenital eye diseases
The human eye forms through a complex process during embryonic development. Problems in this process can lead to congenital (present at birth) eye malformations, such as anophthalmia (no eye), microphthalmia (small eye), coloboma (failure of the optic fissure to close), aniridia (absent or partial iris), and optic nerve hypoplasia (underdeveloped optic nerve). Congenital eye conditions are relatively rare, occurring in approximately five per 10,000 live births.12
Causes of congenital eye diseases
Some congenital eye diseases are passed on through genes, while others can be a result of disease or deficiency during pregnancy. See the descriptions below:

Symptoms of congenital eye diseases
Symptoms of congenital eye diseases include an abnormal-looking eye(s) and reduced vision. They are usually apparent in an eye examination but a patient may occasionally require further tests, such as eye imaging, MRI, CT scan or ultrasounds.15
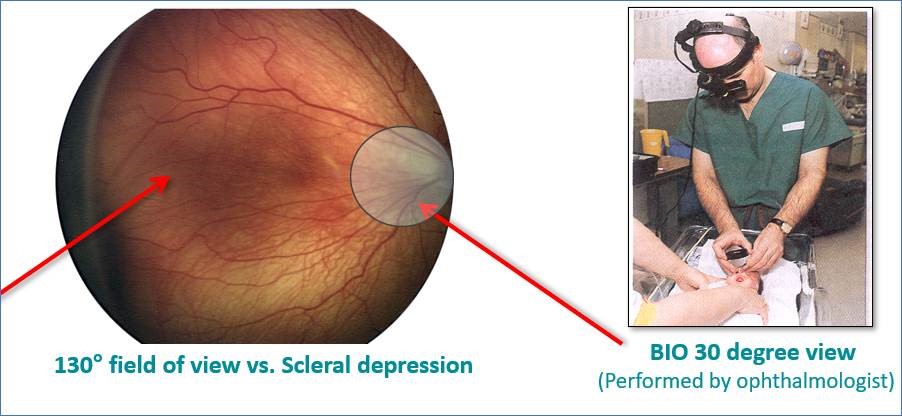 One of the most common ophthalmic instruments used to detect pediatric retinal diseases is a binocular indirect ophthalmoscope (BIO). The BIO is mounted on the head of the Ophthalmologist and provides a view of the inside of the eye through a magnified lens. It allows observation of the retina by moving the BIO device, lens, and applying scleral depression.16
One of the most common ophthalmic instruments used to detect pediatric retinal diseases is a binocular indirect ophthalmoscope (BIO). The BIO is mounted on the head of the Ophthalmologist and provides a view of the inside of the eye through a magnified lens. It allows observation of the retina by moving the BIO device, lens, and applying scleral depression.16
Traditionally, this can be a time-consuming process involving an on-site visit from an Ophthalmologist. Screening can be achieved effectively and efficiently with the use of digital eye imaging in conjunction with telemedicine. In addition, certain conditions require external imaging of the eye for documentation purpose such as anopthalmia or micropthalmia which again can easily be captured with digital imaging.

Digital eye imaging for ROP in the NICU is very easy to perform at the bedside on a baby by a suitably trained NICU staff, and systems like RetCam deliver a full 130-degree view, while BIO provides a 30-degree view17. Using digital images instead of hand-drawn documentation from human memory allows for objective determination of disease state and progression. In addition, the ability to share images with other attending physicians for second opinions improves the accuracy of exams and diagnosis.
Accordingly, digital eye imaging plays a very important role in helping ophthalmologists and attending physicians. Digital eye imaging offers the ease of documentation and the ability to send images for second opinion or referral. In addition to allowing NICU staff to use resources more efficiently, digital eye imaging allows ROP providers to overcome geographical limitations and make timely decisions for infant eye health. In retinoblastoma patients, digital eye imaging can facilitate physicians in grading tumors and allow timely treatment plans for the best possible outcomes. Retinal images also allow physicians to follow the tumor for any growth as well as compare images throughout treatment phases. The digital visualization of pediatric retinal diseases also serves as an educational tool for physicians as well as the infant’s parents or guardians enabling better patient care.
References:
1. https://healthcare.utah.edu/moran/ophthalmology/pediatric/pediatric-retina.php
2. https://childrensnational.org/visit/conditions-and-treatments/eye-conditions/retinal-disorders
3. https://www.cancer.org/cancer/retinoblastoma/about/key-statistics.html
4. https://www.cancer.org/cancer/retinoblastoma/causes-risks-prevention/what-causes.html
7. https://www.cancer.org/cancer/retinoblastoma/detection-diagnosis-staging/signs-and-symptoms.html,
9. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinopathy-prematurity,
11. https://www.childrenshospital.org/conditions-and-treatments/conditions/r/retinopathy-of-prematurity-rop/symptoms-and-causes
12. Pediatric Congenital/Developmental Anomalies Affecting the Eye and Orbit – Conditions and Treatments | Children’s National Hospital (childrensnational.org)
13. https://en.wikipedia.org/wiki/Congenital_cataract
14. https://www.mayoclinic.org/diseases-conditions/toxoplasmosis/symptoms-causes/syc-20356249
15. https://childrensnational.org/visit/conditions-and-treatments/eye-conditions/congenital-developmental-anomalies-affecting-the-eye-and-orbit
16. Binocular Indirect Ophthalmoscopy. EyeWiki, 2 Oct. 2019, https://eyewiki.aao.org/Binocular_Indirect_Ophthalmoscopy
17. Binocular Indirect Ophthalmoscopy. EyeWiki, 2 Oct. 2019, eyewiki.aao.org/Binocular_Indirect_Ophthalmoscopy.
036283 RevA